Meet Laura Matsen Ko, orthopedic surgeon, avid runner/skier/hiker/cyclist, and new mother to a beautiful baby boy, Logan. Laura and her husband, both orthopedic surgeons at Orthopedic Physician Associates (opaortho.com), practice and adventure in the Pacific Northwest. Together, they developed the website, seattlejointsurgeons.com, which allows patients to access comprehensive and accurate information on orthopedic care.
I met Laura recently on Instagram via a post shared by Oiselle (oiselle.com), a Seattle-based women’s running apparel store named after the French word for bird. In the post, photographed by Kevin, Laura is captured as a pregnant backcountry skier posed on the summit of snowy Mt. Baker. A flurry of follow requests, instant messages, and emails between us quickly snowballed into a cross-country friendship. Our easy rapport is not unexpected considering our shared passions. We are both passionate about helping injured athletes (and specifically pregnant athletes) get back to their sports as soon as possible. After learning of my research interests in antenatal exercise, Laura agreed to a semi-formal interview about her background and experiences related to exercise during pregnancy.
First, tell me a little about yourself. I did some Instagram sleuthing and noted scrubs, ortho, a lot of snow, and Thomas Jefferson.
I was born and raised in Seattle, Washington. I went to Whitman College in Walla Walla, WA where I enjoyed being an outdoor leader on backcountry ski trips and mountaineering trips. My senior year I decided to go out for Cross-Country, and surprised myself by placing 9th at Nationals (D3). Then I bike raced that spring and got 2nd at Nationals (D2). That was a huge surprise and a thrill.
I went to medical school in Portland, Oregon at Oregon Health and Sciences University (OHSU) and continued on at OHSU in an Orthopedic Surgery residency. I did two Ironmans while I was there, including qualifying for, and finishing, the world championship in Kona, HI.
About that time I got to meet my husband who was a year behind me in the Orthopedic Residency, and I finally convinced him to go for a real date with me after one of our rainy runs together. Throughout residency we trained for various marathons together and enjoyed active vacations; anything from cycling to backcountry skiing.
After we finished residency, we headed to Philadelphia. I did a fellowship in Adult Reconstruction. I chose the field of hip and knee joint replacement surgery because it gives me the opportunity to help people return to the activities they enjoy using surgery and personalized rehabilitation.
How many years have you been a backcountry skier and mountaineer?
My father and older brother taught me in my teenage years. We had been backpacking our whole lives, they had been climbing, and I always aspired to go out with them. When I was 13 I took a year-long course with my Dad to learn how to safely rock climb, mountaineer, snow camp, and manage avalanche risk and rescue. That winter my brother took me out in the backcountry and I got stronger and smarter. That summer we climbed five Washington volcanic peaks including Mt Rainier.
What kind of role does skiing have in your life?
Backcountry skiing is a wonderful treat—unlike running it does take a bit of equipment and a bit of driving but it’s totally worth it! I love getting out into the wilderness without anyone around. I equally love the hiking up (“skinning” up) the mountain as much as the fresh, sweet turns on the way down!
Tell me about your pregnancy.
Logan was my first pregnancy. I have always been active, and continuing my activity seemed right to me. I bike-commuted to my work at the hospital, rain or shine, which was about a 15-mile commute. I did this through my second trimester, and then we decided it was too high of a risk to continue cycling due to the short and often rainy dark days in Seattle. My OB, husband, and father all pushed me to stop bike-commuting. I ran up to two weeks prior to him being born. I skied two days before he was born—in bounds alpine one day and three days of very rigorous backcountry skiing. These were about 6 hour days of hiking hard uphill and then skiing down in fresh powder. It was so fun to feel like I was sharing this experience with Logan.



The day I went into labor I did elliptical and weights and performed a major total hip revision surgery. Throughout the second half of my pregnancy I had some issues with SI joint and foot pain, but in general my body held up well.
I did a lot of research about heart rates, but the data seemed inconsistent.
Laura’s difficulty navigating antenatal exercise guidelines is not surprising. A study by Lieferman (2012) demonstrated that almost half of medical providers (48%, N=89) were unfamiliar with current national exercise guidelines for pregnant women and half of respondents advised a reduction in exercise in the third trimester, even for uncomplicated pregnancies. Concurrently, a 2006 study demonstrated that about half of surveyed obstetricians recommended heart rate maximums and a reduction in exercise load during the third trimester—two policies not specified in current guidelines (Entin, 2006).
The American College of Obstetrics and Gynecology (ACOG) and the U.S. Department of Health and Human Services recommend that healthy pregnant and post-partum women engage in 30 minutes of moderate intensity exercise for most, if not all, days of the week (ACOG, 2015; DHHS, 2008). Pregnant women who habitually perform vigorous-intensity aerobic activity may engage in higher intensities under the guidance of a medical provider. Heart rate maximums are no longer indicated. Instead, pregnant women use ratings of perceived exertion to monitor their exercise intensity. For most women, moderate effort is comparable to a brisk walk, at an intensity one can maintain for hours. It should result in heavy breathing, but not so much that the exerciser is unable to hold a short conversation. Vigorous activity, on the other hand, should make the exerciser feel short of breath, but still able to speak a sentence.
Obstetrics (OB) providers are encouraged to educate women about the health benefits of exercise during pregnancy. These benefits include improved gestational diabetes control, lower rates of antenatal and post-partum depression, and relief for back pain. There are several absolute contraindications to exercise during pregnancy, including incompetent cervix or cerclage, multiple gestation at risk of premature labor, persistent second- or third-trimester bleeding, and preeclampsia. For a full list of absolute and relative contraindications, consult the ACOG Committee Opinion Number 650 (ACOG 2015). Certain activities are also identified as safe or unsafe. Unbeknownst by Laura, down-hill snow skiing is listed as an activity to avoid due to an inherently high risk of falling and subsequent abdominal trauma.
Laura continues:
I didn’t really follow [the guidelines] after talking with friends and reading. I didn’t do sustained high intensity intervals, but if I was running stairs and my heart rate got up to 165-170 on the way up but dropped to 120 on the way down, I felt that my baby was getting sufficient perfusion. Each mother has a different pregnancy experience and the biggest factor is to listen to your body. Exercise made me feel happy and alive so I kept doing it. Plus pregnancy can do such a warp on body image. Exercise helped normalize my feelings about the changes in my body.
Why do you think it is most important to listen to your body?
We are all so different. As you’ve seen with your med student classmates, we need different amounts of sleep, caffeine, food, exercise, fresh air… so no single guideline will work. We all must strive to learn our bodies.
My physician friend had a 10-lb baby. She was extremely active, and pre-pregnancy she ran and played soccer. Obviously our pregnancy (and delivery and post-partum) experiences were totally different and not fair to compare. She says she tried to play soccer 7 weeks post-partum and she “felt like her uterus was going to fall out.” Another physician friend had a 9 lb baby with a very large head. She was walking over 5 miles a day until she delivered, but is challenged to get back to walking more than a couple blocks now (2 weeks post-partum) after her more traumatic vaginal delivery. A third physician friend who had always been extremely active in basketball and volleyball was placed on bed rest at 22 weeks for all three of her babies.
I never want to be compared to other women or make other women feel that they just didn’t push hard enough because of my activity levels. I’m one person and this was one pregnancy. The next pregnancy could be totally different! These other women are a lot tougher than me—they had a more challenging pregnancy, delivery, and recovery. And they had to be very patient with their bodies.
Did you have any conversations with your OB provider(s) about your exercise practices during the pregnancy?
Yes… some. They thought I was a little nuts but were supportive. Except for the skiing. My OB was a little shocked to hear that I’d been skiing.
In the first couple weeks post-partum I mostly tried to work on some baseline fitness with walking and stairs. I tried to wait until 6 weeks to really increase my activity but I wasn’t able to wait.
Explain the 6 week mark.
Well I was told by my OB and the nurse practitioners to not exercise hard until 6 weeks. BUT I started running at day 16 and as of 4 weeks was up to about 30-40 miles a week with one day of hill repeats and one day of fartleks. I made it to 8 miles in sub 8 pace with a couple 7:30 until around 4 weeks. I think my first race will be a half marathon at 2.5 months postpartum. I’m not going to be the fastest. Partly because of recent pregnancy but also because of sleep deprivation, returning to work, and not having enough time in the day!

Do you have any friends who also skied during their pregnancy?
I knew people who were running and rock climbing in their pregnancy and a lot of friends who just stayed fit with walking. I don’t know anyone else who skied during their pregnancy but I’m sure people out there do it! I’d mainly suggest borrowing your father’s huge rain coat and possibly his ski pants because there is no way you’re fitting in your bibs from pre-pregnancy. And don’t push the speed and steepness; mostly enjoy being out there! You don’t want to fall.
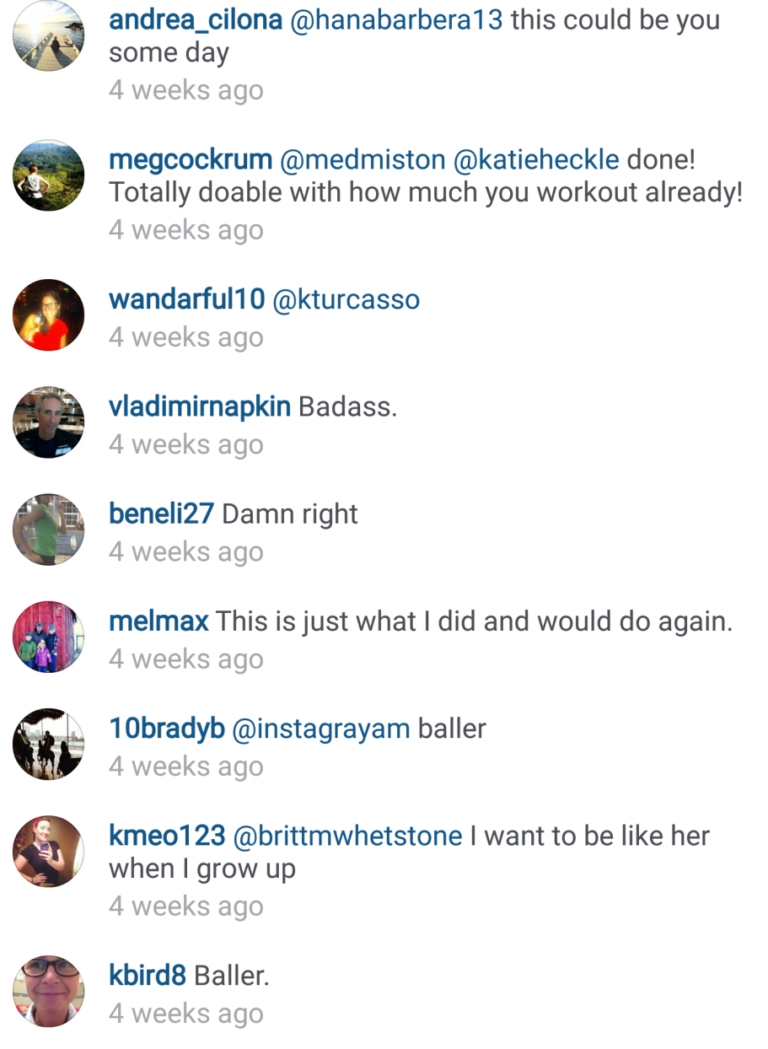
There are definitely other pregnant skiers and a few inspired, future Mamas:
On the mountaineering trips, what, if any, issues did you have with harness fit?
Due to the season I didn’t mountaineer in the second half of pregnancy, so it wasn’t an issue. One of my friends got a lower and upper body harness for her pregnant rock climbing trips.
What kinds of emotions did you encounter during your pregnancy when you were not able to do activities that you enjoy?
I found it super frustrating when others placed restrictions on me. My husband quickly found that he had to present my change in activities as a risk/ benefit. When he told me “no more cycling,” I just wanted to rebel. However he did recently have to fix a clavicle fracture on a woman who was 16 weeks pregnant. She got hit while bike commuting. Thankfully her fetus is okay. That story will make me more conservative with my cycling in my next pregnancy.
At 4.5 weeks post-partum I restarted bike-commuting to work for some half days of clinic. It felt amazing to be back out there and I was so much faster with less weight, higher lung capacity, and likely an increased hematocrit.
Is there anything you want to tell future mothers?
Listen to your body and don’t read too much. Wear support stockings if you work on your feet. Know that you will lose the weight. Fast.
Physicians?
Support your patients.
For future and current obstetrics providers, the Canadian Society for Exercise Physiology developed the PARmed-X for Pregnancy, a physical activity readiness medical questionnaire that guides discussions on exercise during pregnancy in an outpatient setting. The form may be accessed online (http://www.csep.ca/cmfiles/publications/parq/parmed-xpreg.pdf) and is useful for most pregnant women. Athletes, however, have sport-specific safety concerns, training goals, and requirements that may be unfamiliar to the average obstetrics provider. These topics may be explored on an as-needed basis during prenatal visits.
A big thank you to Laura Matsen Ko for sharing your inspiring story! Thank you also to my friend Hannah, who initially tagged me in the Oiselle Instagram post.
References
- Leiferman, J., Gutilla, M., Paulson, J., Pivarnik, J. (2012). Antenatal physical activity counseling among healthcare providers. Open Journal of Obstetrics and Gynecology, 2, 346-355
- Entin, P. L., Munhall, K. M. (2006). Recommendations regarding exercise during pregnancy made by private/small group practice obstetricians in the USA. J Sports Sci Med, 5, 449-458.
- American College of Obstetricians and Gynecologists. Physical activity and exercise during pregnancy and the postpartum period. Committee Opinion No. 650. Obstet Gynecol 2015;126:e135–42
- U.S. Department of Health and Human Services. 2008 Physical Activity Guidelines for Americans. Department of Health and Human Services Washington, DC; 2008.
Featured image:
Laura Matsen Ko skiing. Photographed by Kevin Ko.


