Surrounding me in the Barcelona airport this past winter was the latest technology—new scanners and gadgets directed at catching radioactive and explosive material more quickly and safely than before. Large plasma screen TVs were on every corner, and numerous retail shops caught my eye at every glance. With an expansive collection of restaurants and shops, one would think this is more of a mall than an airport. Given the mini-mall appearance, I felt I would have no trouble finding a place to purchase a tampon or pad, as Mother Nature had unexpectedly paid me a visit and I was unprepared. After first checking the bathroom for a tampon dispenser and finding none, I went from store to store looking for a personal hygiene section. To my dismay, there were an assortment of shaving creams and toothbrushes and even diapers, but there were no tampons or pads to be found. After scanning all the stores in my immediate vicinity, I decided to inquire at the cashier desk, which was occupied by a female clerk. When I asked her about where I could potentially find some feminine hygiene products, she informed me that I was out of luck. Her and other female colleagues all kept tampons and pads in their bags because there was no place to purchase them in the area. Fortunately for me, they kindly provided me with a few from their stash for my long journey home.
While this may be expected in a less developed area with few resources, an airport that boasts being “among the top 30 busiest airports in the world”1 should have several places to purchase feminine hygiene products. I was incredulous that an airport outside a major hub in Europe in the 21st century had no place for female employees or travelers to purchase a pad or tampon. This is an issue that must be corrected—whether by adding tampon dispensaries or vending machines, or simply by increasing inventory in the numerous retail shops lining the terminals. The Barcelona airport, along with any other major public areas that are traversed daily, should be required to carry these products.
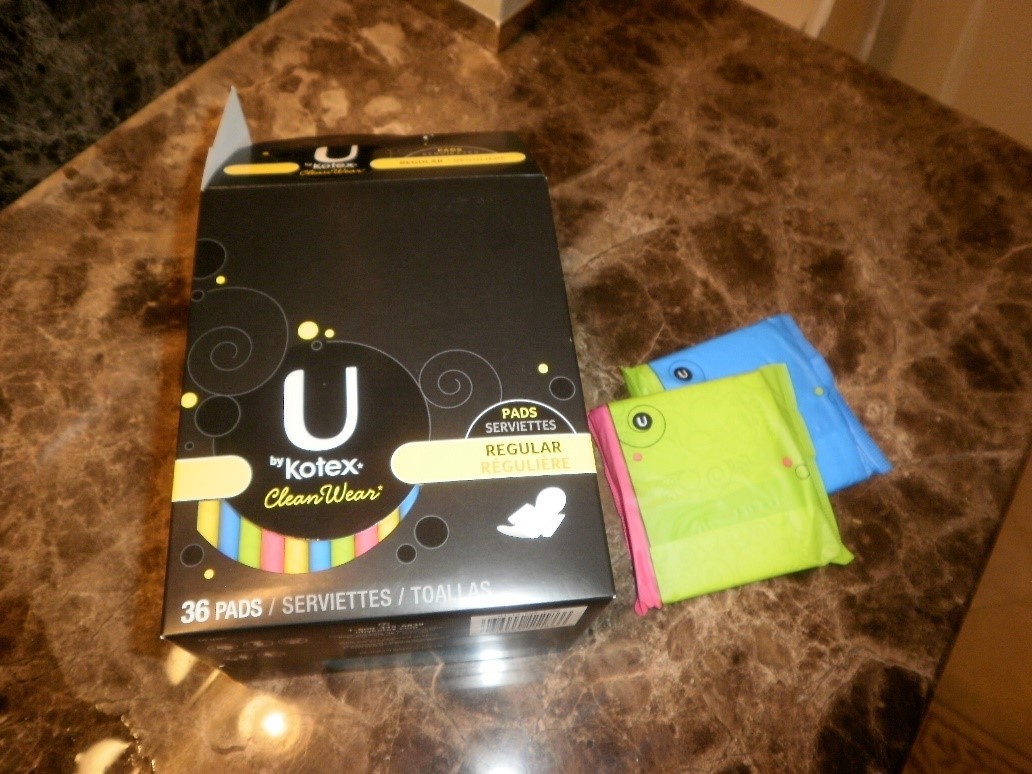
While I was fortunate enough to receive some aid from the female clerks at one of the retail shops, I know there have been many other women who have been inconvenienced by either lack of menstrual products or their cost. In the same month, another traveler at the Calgary YYC airport reported that she had to pay a whopping $15 for a box of tampons at the airport2. Of course, it is a known fact that prices in the airport are always much higher than in retail shops outside – same goes for museum gift shops and others located near tourist attractions. However, for a product that is a basic hygienic necessity for half of the globe’s population, it is prejudicial that it is also priced almost double what it is in a regular grocery store. That traveler’s post sparked a global dialogue as to why these products are not easily found or are not affordable in places that millions of women work or travel.
While a dialogue is an important start, we need to continue to bring this issue into the spotlight. No woman in 2018 should be forced to pay egregious prices for basic hygiene and even more importantly, there should be access to feminine hygiene products in all institutions, including schools, airports, and workplaces.
Source(s):
1https://www.barcelona-airport.com/eng/information.php
2http://www.metronews.ca/news/calgary/2017/12/04/viral-post-blasts-tampon-price-gouging-at-yyc-airport.html
Photo credit: Sor Cyress Source: Flickr